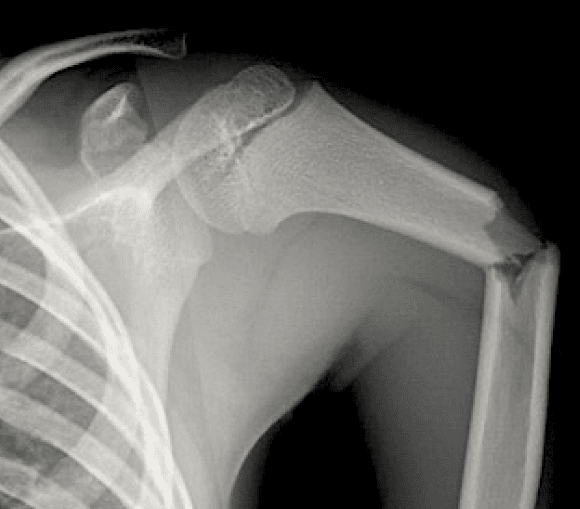
The humeral shaft is defined as the area distal to the surgical neck and proximal to the epicondyles.
The commonality of fracture is:
Middle ⅓ > Proximal ⅓ > Distal ⅓ shaft
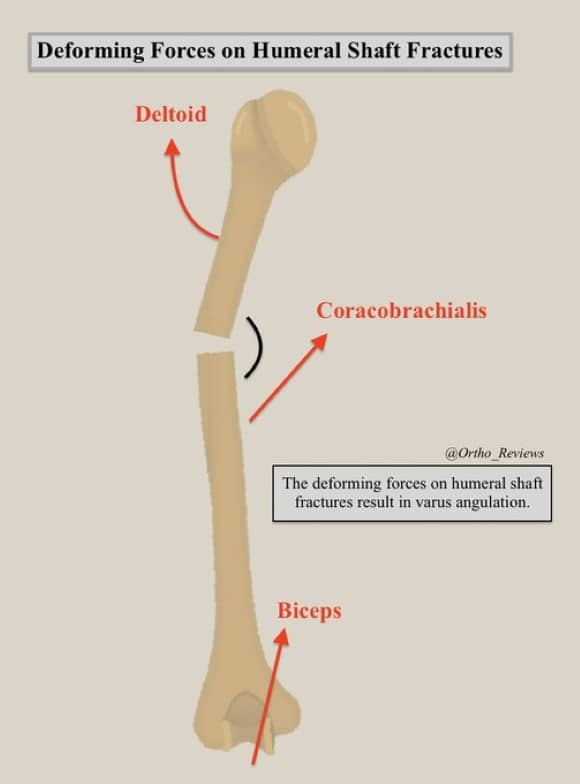
Due to the muscular pull of the deltoid on the proximal fragment and medial/superior pull on the distal fragment, humeral shaft fractures tend to develop varus angulation.
Humeral shaft fractures are forgiving, and modest angulation can be overcome by the shoulder's large ROM.
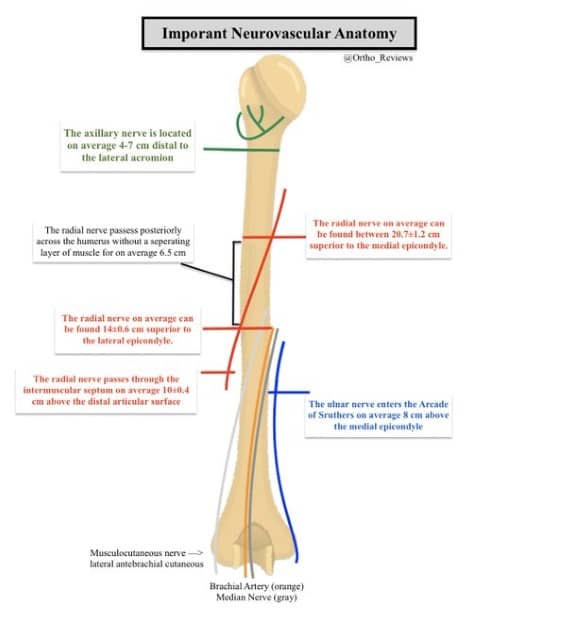
Important neurovascular anatomy:
✯The radial nerve is most commonly injured in humeral shaft fractures
✯It passes across the posterior humerus along the spiral groove over an average distance of 6.5 cm
✯It is most vulnerable to injury as it passes through the IM septum, where it is least mobile
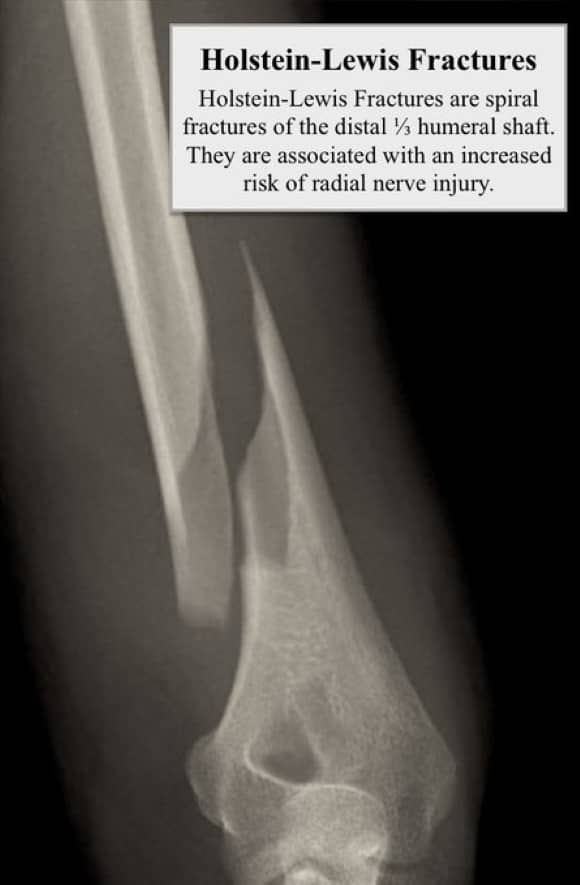
In a 2008 @JofOrthoTrauma study, Ekholm et al again showed that radial nerve palsy was more common in Holstein-Lewis fractures, 6/27 (22%) compared with 27/334 (8%) in other fracture types.
Holstein-Lewis fractures account for 3.8-7.5% of humeral shaft fractures.
The majority of humeral shaft fractures can be managed non-operatively, though patient and fracture characteristics must be taken into account.
Though there has been a recent uptrend in surgical management of humeral shaft fractures, as noted in a 2017 study by Schoch et al.
Treatment considerations:
✯ Non-operative tx requires close follow-up
✯ Large body habitus & pendulous breasts may pose a challenge for maintaining alignment
✯ Anticipated return to work/activities
✯ Both non-operative and operative treatment are associated with complications
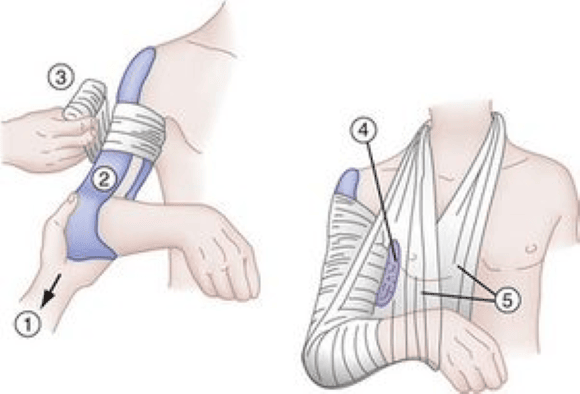
The first step in the management of most humeral shaft fractures is reduction and placement in a coaptation splint.
A valgus mold should be induced to counteract varus deforming forces.
It is important to perform a pre- and post-reduction neurovascular exam.
In a 1966 @jbjs study Klenerman et al established a set of non-operative tolerances for humeral shaft fractures:
✯ <30° coronal angulation (varus/valgus)
✯ <20° sagittal angulation (ant./post.)
These parameters are still commonly used today for guiding treatment.
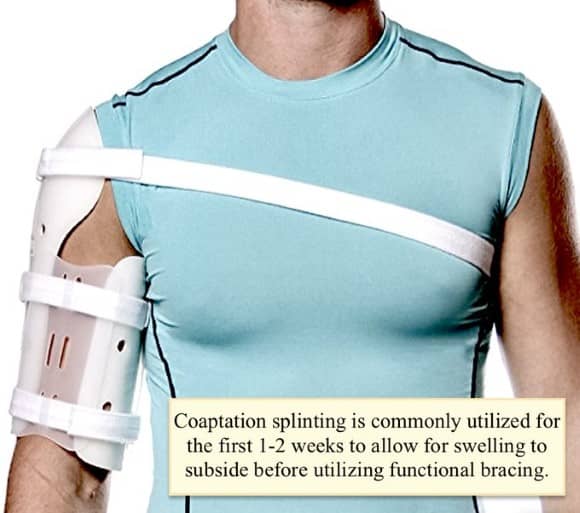
Following their 1997 study in @jbjs Sarmiento et al popularized the use of functional bracing as a non-operative treatment for humeral shaft fractures.
Commonly termed: Sarmiento bracing
It works by compressing soft tissues and utilizing hydrostatic forces to maintain reduction
Operative indications:
✯ > 30° Coronal angulation
✯ > 20° Sagittal angulation
✯ > 3 cm shortening
✯ Intra-articular extension (spiral fx)
✯ Vascular Injury
✯ Floating Elbow
✯ Segmental Fracture
Surgical options include ORIF with plate/screws and intramedullary nailing.
There have been many recent studies comparing the outcomes and complications of plate osteosynthesis vs. intramedullary nailing.
Recent studies have shown similar union rates, though complication rates (e.g. shoulder pain) may be higher with intramedullary nailing.

Complications:
Radial Nerve Palsy: most patients experience spontaneous recovery within 6 months and when to perform surgical exploration has been a topic of debate
Malunion: most patients tolerate moderate angulation without clinical significance
References:
1: https://pubmed.ncbi.nlm.nih.gov/873955/
2: https://pubmed.ncbi.nlm.nih.gov/28484909/
3: https://pubmed.ncbi.nlm.nih.gov/29292035/
4: https://pubmed.ncbi.nlm.nih.gov/5909054/
5: https://pubmed.ncbi.nlm.nih.gov/18836600/
6: https://pubmed.ncbi.nlm.nih.gov/18978544/
7: https://pubmed.ncbi.nlm.nih.gov/8934483/